Overall Goals
Women are at twice the risk of men for the co-occurrence of major depression, autonomic dysregulation, and cardiovascular disease (CVD) risk. Study aims are to:
Investigate early (fetal) antecedents to the co-occurrence of major depression, autonomic dysregulation, and CVD.
Identify stress and immune factors that are dysregulated during prenatal development that differentially impact male and female offspring and their risk for major depressive disorder, stress/mood circuitry in the brain, and associated impact on cardiac physiology and neurovascular function in early midlife.
Identify early biomarkers for the co-occurrence of depression and CVD risk that will provide knowledge to intervene earlier in a sex-dependent way.
Specific Aims
Aim 1
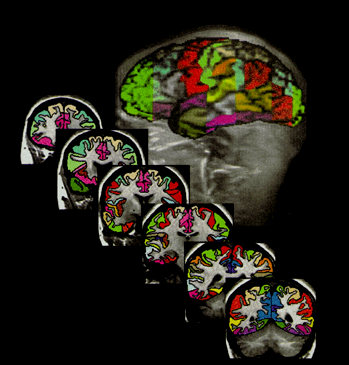
Use multi-modal imaging to characterize sex differences in neurobiology, ANS, immune, and steroid hormone physiology & neurovascular dysfunction associated with stress response circuitry deficits in recurrent depression vs. healthy controls.
Aim 2
Test whether and how adverse prenatal maternal immune exposures are significantly associated with deficits found in Aim 1.
Aim 3
Test whether abnormalities in offspring gene expression in inflammatory pathways, using transcriptomic analyses of offspring peripheral blood mononuclear cells (PBMCs), is associated with maternal prenatal immune exposures, providing potential mechanism for the enduring sex-dependent effects of prenatal immune exposure.
Our Senior Team
Key Discoveries by Our Team
Significant sex differences in how we regulate stress in the healthy brain are associated with gonadal hormone regulation of the brain. (Goldstein et al, 2010)
Sex differences in the healthy brain are dysregulated in major depression. (Jacobs et al, 2014; Mareckova et al., 2016)
Sex differences in regulation of stress are shared across psychiatric disorders as depressed mood increases. (Mareckova et al., 2016)
Stress is associated with numerous chronic diseases, beginning in fetal development wherein in utero exposures impact offspring’s risk for disorders later in life. (Goldstein et al., 2018)
Prenatal exposure to pro-inflammatory cytokines increases risk for the co-occurrence of major depressive disorder and cardiovascular risk. (Gilman et al., 2016; Goldstein et al., 2018)
Prenatal maternal exposure to TNF-a:IL-10 had long-standing sex-dependent impact on offspring stress response circuitry deficits in hippocampal activity and connectivity between hypothalamus and hippocampus 45 years later. (Goldstein et al., 2021)
In the largest genome-wide genotype by sex analysis of mood and psychotic disorders to date, shows substantial genetic overlap between the sexes exists. However, significant sex-dependent effects were enriched for genes related to neuronal development, immune and vascular functions across and within disorders at the variant, gene, and pathway enrichment levels. (Blokland et al., 2021, Biological Psychiatry)